Revolutionary TOGAF ADM process and development tools designed for all EA teams.

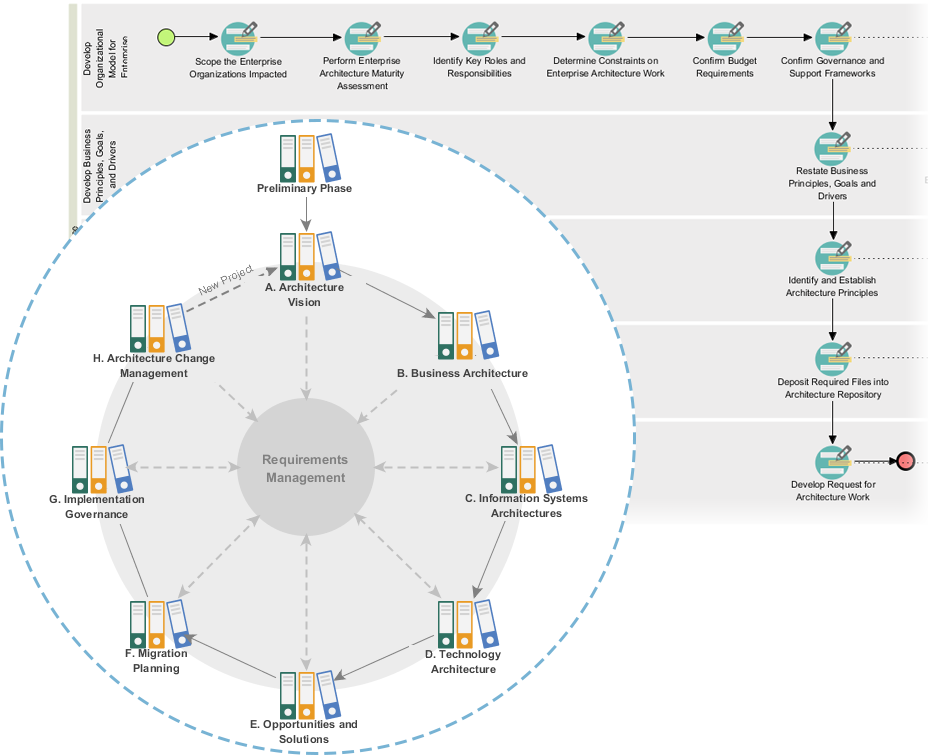
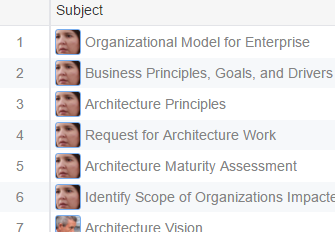
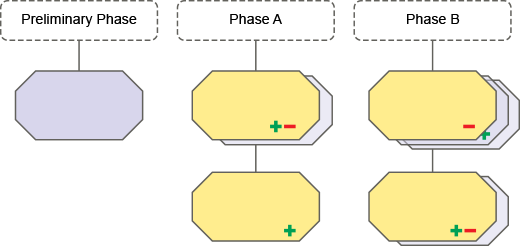
The TOGAF ADM phases and steps are visualized as a stack of visual process maps, which helps you navigate through the entire EA process easily.
Full set of planning, design and development tools are provided for you to complete the ADM activities. Just double-click on an activity to access the tools and start working on the activity. Instructions and examples are provided to help you understand TOGAF and to complete the actions effortlessly.
As said, you are provided all the EA tools you need to complete the ADM activities. These include mostly design and modeling tools for creating visual models, and matrixes for inputting listed data. Listed below are some of the tools we provide.
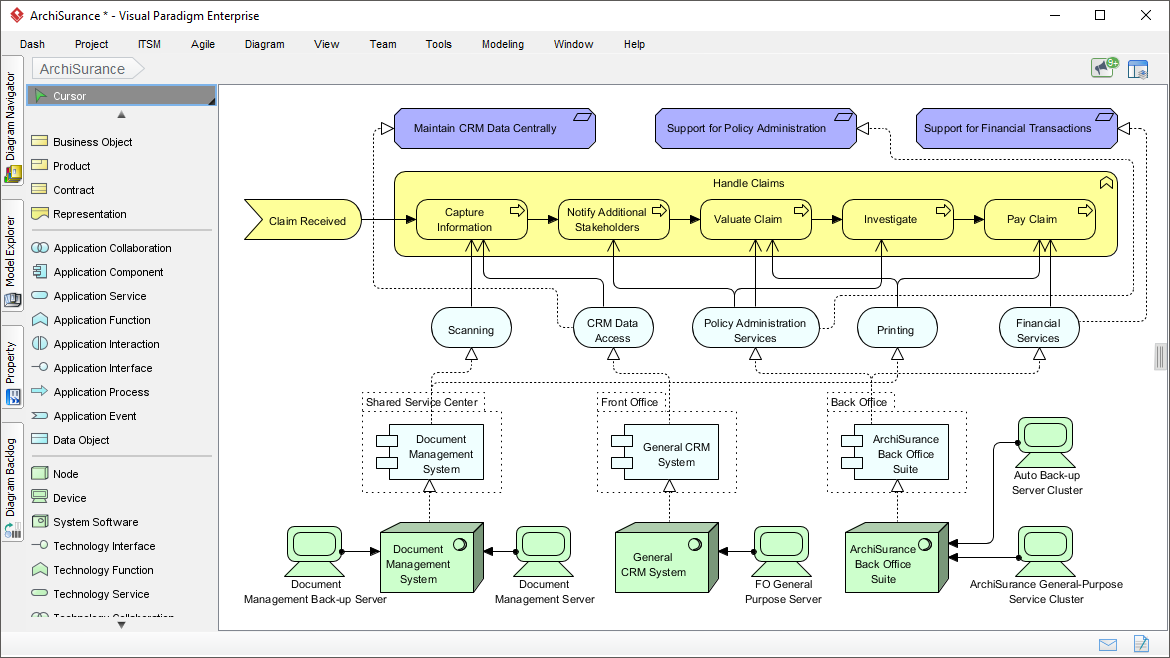
Model the business, IT and physical aspects of your enterprise architecture with ArchiMate diagram
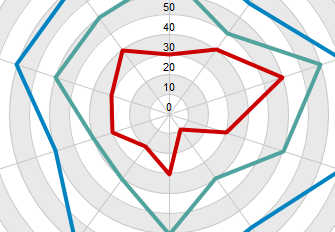
Use radar chart for maturity analysis and capability assessment
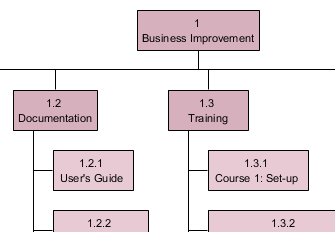
Model your team and project structure with breakdown structure diagram
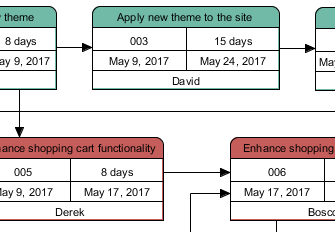
Create pert chart for showing the milestones of your EA project(s)
Manage project tasks with a powerful task management platform
Define and describe your EA plan in a handy fill-in-the-blank manner
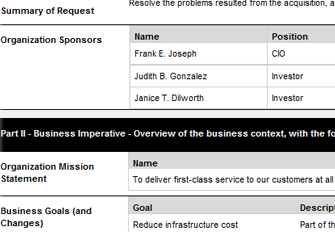
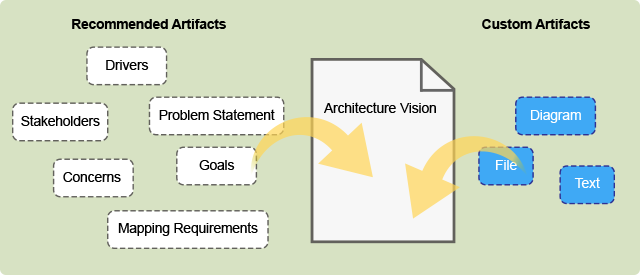
As you complete the activities, artifacts are gradually developed. Artifacts are reused throughout the entire ADM process, meaning that your work created earlier will be populated in subsequent activities. You just need to enrich the artifact activity to activity, phase to phase. No re-work is needed.
Your work will be extracted and arranged to create TOGAF ADM deliverables (i.e. reports). You just need a click to get a deliverable generated. No touch-up is needed. But if you want you can still customize the deliverable to suit your need. A full-featured report editor is available for easy customization.
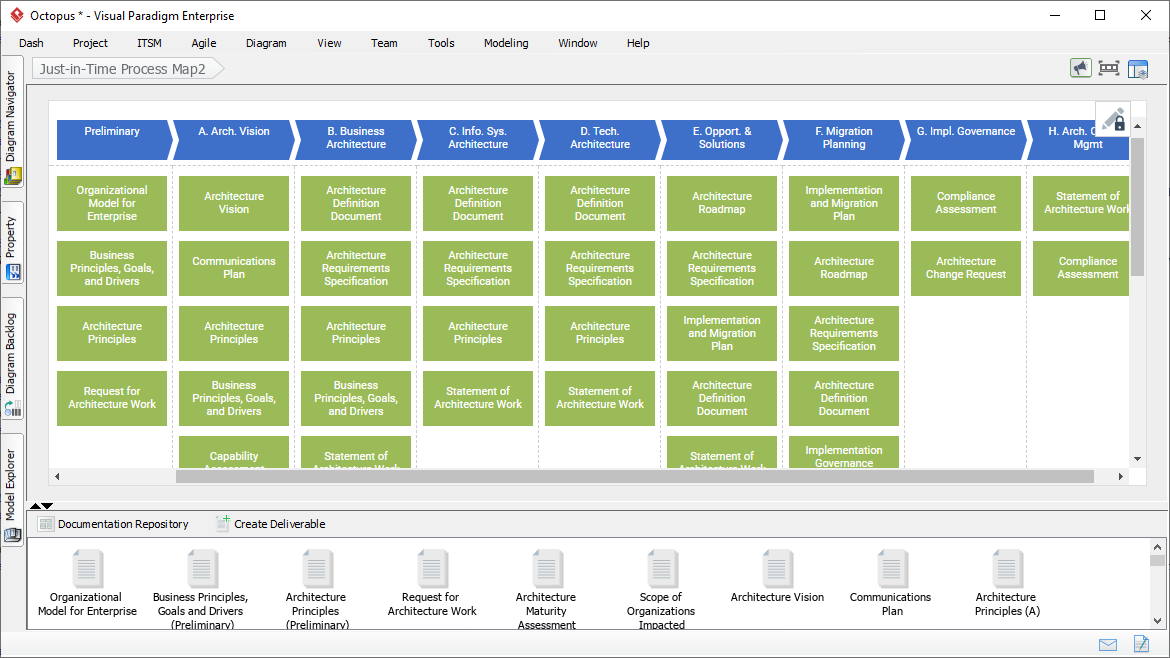
Besides the visual ADM process maps, Visual Paradigm also features a highly configurable TOGAF ADM process map. The map contains all the actionable work items your team need to design, plan, develop and govern an enterprise collaboratively using TOGAF ADM. Enterprise architects follow the steps and instructions defined in each work item to get the architecture developed. Deliverables will be automatically generated and archived in Architecture Repository, a visual File Cabinet.
Create professional enterprise architecture blueprint quickly and collaboratively using an ArchiMate software chosen by enterprises from all over the world. Certified by The Open Group, Visual Paradigm features an ArchiMate modeling tool that is targeted toward all levels of enterprise architects and enterprise modelers, supporting architecture design needs with all the vocabulary, notation, syntax, and semantics of the ArchiMate 3.1.